
Two Looming Crises Threaten to Collapse U.S. Long-Term Care
Immigration Crackdown and Medicaid Cuts Put Millions at Risk
Penn LDI and Tradeoffs present “Decoding the Moment” – a virtual event series offering timely, evidence-based discussions on major federal policy changes with leading experts. Join the discussion about the impact of recent actions and what they mean for the future.

Our work addresses some of the most pressing health and health care challenges facing our nation today.

In Their Own Words
Health Care Access & Coverage
Immigration Crackdown and Medicaid Cuts Put Millions at Risk

In Their Own Words
Health Care Access & Coverage
Will This Time be Different? Past Health Bills Hold Clues

Blog Post
The Inflation-Adjusted NIH Budget is Lower in 2024 Than It Was at Its 2003 Peak

Policy
Health Care Access & Coverage
Supplement to Response to Request for Technical Assistance

In Their Own Words
But Many Other Factors Played a Role in Denying Loans, LDI Fellow Says

Blog Post
A Simple Change to Clinicians’ Prescribing System Reduced Prescription Disparities by Race, Ethnicity, Insurance Type, and Income

Virtual Event
Presented by Penn LDI and Tradeoffs

Our Fellows are featured in leading local and national outlets – including The Washington Post, STAT News, Newsweek, and more – sharing research and insights that shape conversations on health policy, health care delivery, and population health across the country.
In The Media MedPage Today
Interview
In The Media The New York Times
Interview
In The Media Fortune
Interview
In The Media Fortune
Interview
In The Media EurekAlert!
Interview
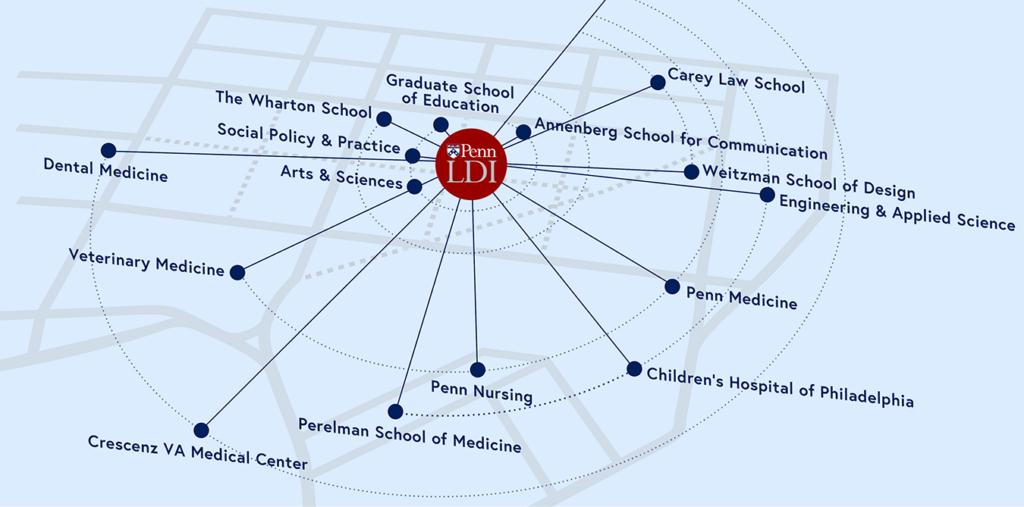
Our 500+ Fellows are national experts and thought leaders who bridge all of Penn’s schools, the University of Pennsylvania Health System, and the Children’s Hospital of Philadelphia.








As Penn’s hub for health care delivery, health policy, and population health, we connect and amplify over 500 Fellows across the University, and train the next generation of researchers.
$160M+
Awarded in External Grant Funding
11,300+
Journal Articles Published (2020–2024)
$400K+
Awarded in Research Grants from LDI